If you have experienced foot pain, you’ll understand how debilitating it can be. It can cause you to dread your weekly morning run, workout class or even getting out of bed. With many athletes training for the Philadelphia Marathon in November we thought it’d be a perfect time to educate on the most common type of foot pain – plantar fasciitis – and how to fix it.
Let’s break it down…
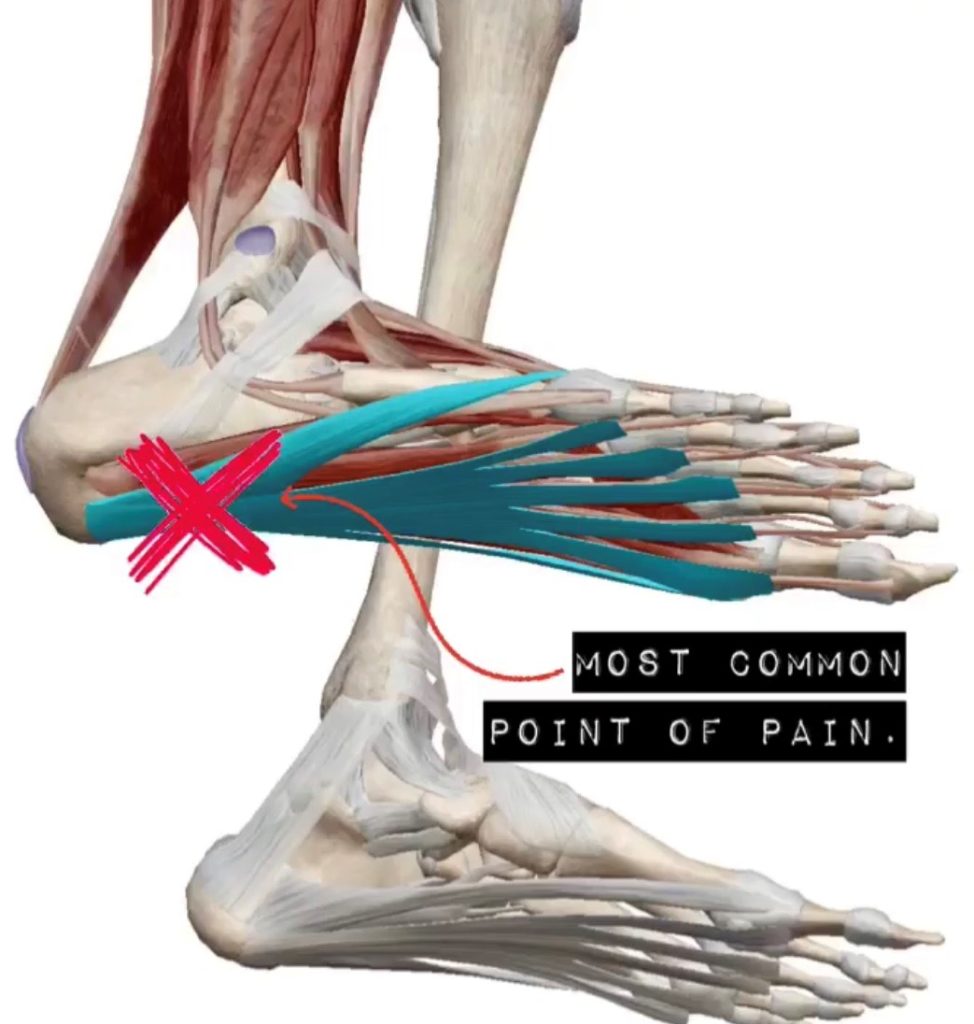
Plantar fasciitis is inflammation of the plantar fascia – the thick fibrous band of tissue that runs along the bottom of the foot. More specifically, the inflammation usually occurs at the medial (or inside) aspect closest to the heel. It is most often described as a “sharp” pain that radiates along the bottom of the inside of the foot. “It feels like stepping on glass” is what we hear most often when patients describe their pain. This pain is noticeably worse in the morning when taking those first steps (no need for coffee, that is one way to wake you up in the morning) or with weighting the foot after a period of inactivity.
How do I get Plantar Fasciitis?
Certain activities increase the likelihood of developing plantar fasciitis such as long-distance running, and ballistic jumping activities seen in high intensity workouts and dancing. Additionally, if an athlete has a sudden increase in distance, duration, or intensity of activity they are more prone to develop plantar fasciitis.
Poor quality or old shoes, and/or running on hard surfaces leads to more wear and tear on the plantar fascia over time. Wearing the proper footwear for your activity is crucial. Runners need running shoes. Weightlifters need lifting shoes. We have seen many patients come in with foot pain after wearing the wrong shoes – even just once.
Another risk factor involves prolonged standing/walking. More weight placed on the plantar fascia over an extended time increases the likelihood of developing plantar fasciitis. Occupations such as teaching or nursing lead to more instances of plantar fasciitis.
The research shows that people with low arches (“flat feet”) are more likely to develop plantar fasciitis with over pronation (rolling inward). The research also shows that people with high arches develop foot pain with increased activity. The bottom line is anyone can develop foot pain. You are likely to develop pain if you are flat footed or have high arches, if you are bouncing around a lot or standing all day. The bottom line is you need to get it fixed.
Enough with how it happens let’s talk about how we can fix it!
It has been found that “95% of patients respond to conservative care” when it comes to foot pain (Souza, 2016). Conservative care includes myofascial release of the plantar fascia & calf muscles and addressing biomechanical dysfunctions & joint restrictions of the foot, ankle, knee and pelvis. Taping can provide temporary support of the foot and decrease pressure on the plantar fascia, but typically is more effective if accompanied by gradual stretching and strengthening of the foot musculature.
What kind of stretches can I do to help relieve the pain?!
We recommend stretching before you get out of bed in the morning by keeping a towel or TheraBand beside your bed. Before you get up, wrap the towel/TheraBand around the forefoot and pull with both hands to cause a passive stretch of both the plantar fascia, Achilles tendon and calf musculature. See image below.

Morning Towel Stretch – With the towel wrapped around the forefoot pull with both hands to cause a passive stretch to the plantar fascia, Achilles tendon and calf musculature.
Another helpful tool is a lacrosse ball. Rolling the foot on top of a lacrosse ball to release the fascia is very helpful (uncomfortable but helpful). You can also use a frozen water bottle to roll the foot. This has the added benefit of cooling and reducing the inflammation while releasing the fascia. See this instructional video below to give you more information of how to perform properly.
If you recognize these symptoms and have foot pain, give your friends at Spinal Care a call. We can release the affected tissues and provide a home mobility and strengthening program to get you out of pain and keep you that way.
Reference.
“Differential Diagnosis and Management for the Chiropractor” Souza, T, A. (5th edition; 2016).















































































